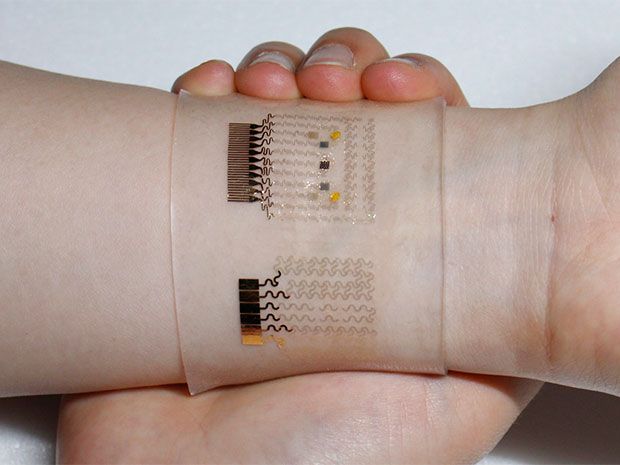
Graphene Wristband Senses Your Blood Sugar--and Treats It
Scientists have unveiled a see-through wrist cuff that measures the level of glucose in the bloodstream of diabetic patients and administers a drug to lower that level if needed. It’s not yet a full-blown treatment—for one thing, the experimental version can’t provide enough of the drug to do the trick—but it should be of great use in monitoring patients.
It’s also an actual application for a newfangled material in sore need of one: graphene, a superthin form of carbon with interesting electronic properties. By itself, graphene can’t sense glucose, but if you dope 2-D carbon properly, it can become quite a useful elecrochemistry set. The inventors—working in South Korea, Massachusetts and Texas—doped the graphene with minute quantities of gold to get the effect they wanted. They describe their work in this week’s issue of the journal Nature.
The idea of replacing the failing function of a diabetic pancreas dates even further back than the isolation of the critical pancreatic hormone insulin, in the 1920s. Before that, doctors had hoped to transplant the pancreas itself, or part of it, but they quickly found that the immune system would reject such a graft. Even with today’s antirejection drugs such transplantation can be problematic because those drugs can have side effects worse than the diabetes itself. Besides, transplantable tissue is in short supply.
That’s why bioengineers have long wanted to devise a mechanical alternative to the organ—a robotic pancreas that would sense and then treat excessively high (or low) glucose levels in the blood. Because such a device handles both the sensing and dosing ends of the feedback loop, it’s called a closed-loop solution.
In the past year or two, the first partially automatic systems—call them semi-closed-loop devices—have hit the market. They are now used only by patients with Type 1 diabetes (or juvenile diabetes) in which the body no longer makes any insulin and so requires that it be injected. Such a robopancreas has a tiny needle that’s inserted under the skin, to detect changes in blood glucose; a computer to figure out what to do; and an insulin pump, which administers insulin through a superthin pipette, also under the skin. The three elements are linked wirelessly.
This method can fail if the sensor takes too long to get an accurate reading or if the hormone takes too long to do its job—a difficulty known as latency. That’s one reason why today’s commercial machines still require that the patient be involved in managing the system, for instance by administering a dose of insulin before a meal.
For Type 2 diabetes, a less severe and far more common form, it may be easier to create a fully automatic closed-loop machine. In this form of the disease, the patient’s pancreas still makes insulin and may merely need a nudge to make more of it. The graphene wristband provides that nudge by supplying metformin, a drug that stimulates the pancreas to make insulin.
The wristband senses a number of things in the patient’s skin—the mechanical strain, the temperature, and above all the chemical composition of the sweat—to infer the level of blood glucose. The researchers report a lag of 15 to 20 minutes between a change in the blood and the corresponding change in the sweat, but the latency may not be too much of a problem for people with Type 2 diabetes.
Next, the wristband shares sensor data wirelessly with a mobile device, which calculates the proper dose of metformin and has the wristband administer it through an array of microneedles. The array goes into action when a current warms it to 41 degrees Celsius (105 °F), which makes you wonder what would happen, say, at high noon in the tropics. But at least the microneedles are unobtrusive enough to call the device minimally invasive—a selling point for needle-shy patients.
The researchers proved that the system can normalize blood sugar in lab experiments on animals. However, though the device has administered metformin to human subjects, it didn’t supply very much of the drug.
“With the present design, it seems extremely unlikely that the daily adult dose of metformin can be delivered without an unfeasibly large number of microneedles and/or an unacceptably large patch,” writes Richard Guy, a researcher in pharmacology at the UK’s University of Bath.
Also, unlike today’s semi-automatic robopancreas devices, the wristband does nothing to correct excessively low blood glucose, which typically comes after overcorrecting the opposite problem. “Nevertheless, it is probably safe to say that these issues are already being addressed and that other therapeutic strategies are being identified to complement the significant advances achieved in this work,” Guy concludes.
Meanwhile, there’s the simple advantage of using a see-through band just as a sensor. With no muss or pain, the band can tell you how much glucose is coursing through your veins and leave it to you to do something about it.




